Renaud Tamisier, Jean-Louis Pépin, Holger Woehrle, Muriel Salvat, Gilles Barone-Rochette, Cécile Rocca, Eik Vettorazzi, Helmut Teschler, Martin Cowie, Patrick Lévy
- Share
- Share on Facebook
- Share on X
- Share on LinkedIn
Abstract
Background
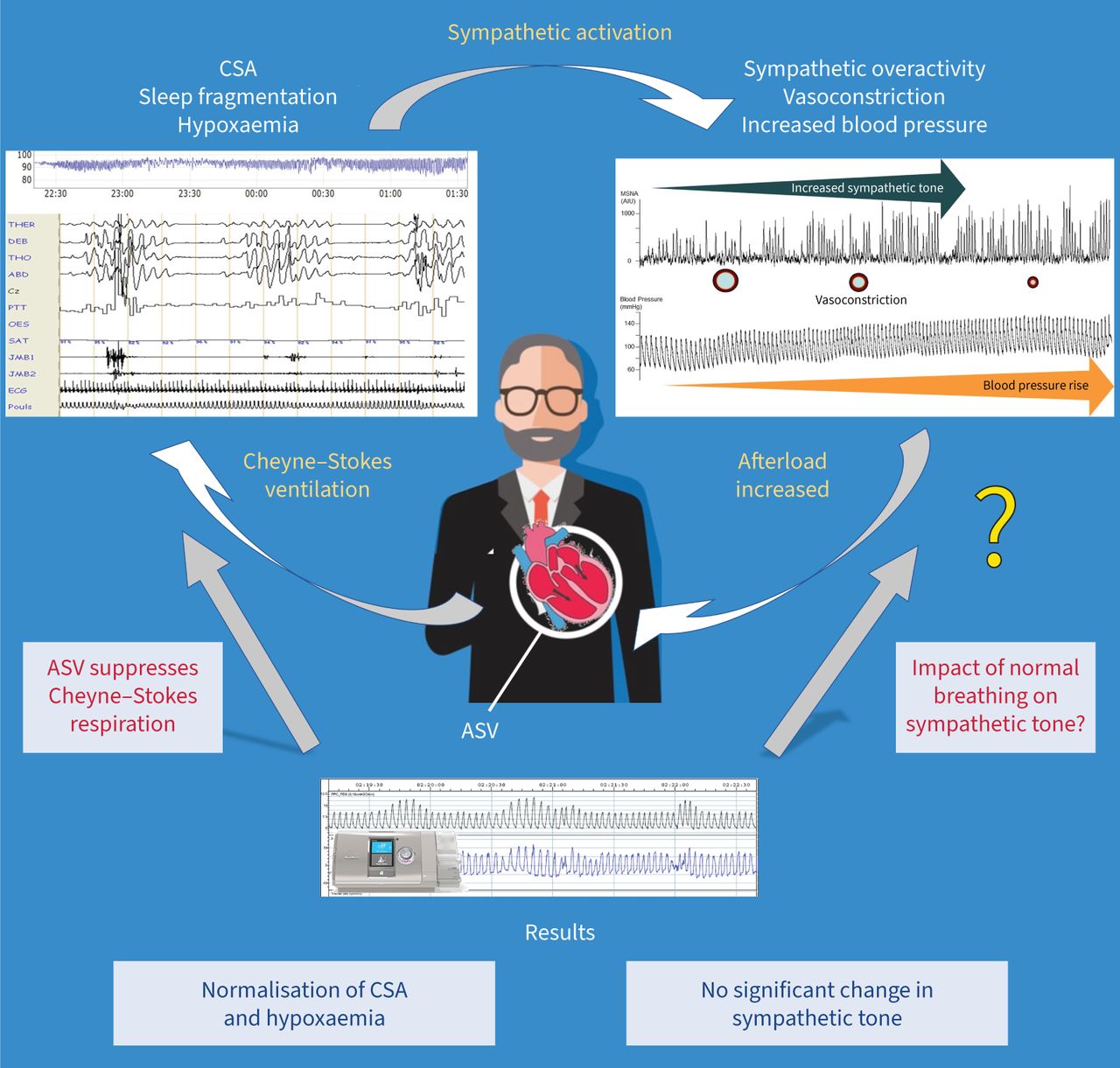
Adaptive servo-ventilation (ASV) effectively suppresses central sleep apnoea (CSA) but has been associated with increased all-cause and cardiovascular mortality in chronic heart failure patients with reduced ventricular ejection fraction (HFrEF). All-cause and, especially, cardiovascular mortality in chronic heart failure is highly correlated with sympathetic tone. This analysis of SERVE-HF data investigated the effect of ASV on sympathetic tone in patients with HFrEF and CSA.
Methods
HFrEF patients in the SERVE-HF trial (left ventricular ejection fraction (LVEF) ≤45%, apnoea–hypopnoea index (AHI) ≥15 events·h−1 with predominant CSA) were randomly assigned to receive guideline-based heart failure treatment alone (controls) or plus ASV. For this analysis, the primary outcome was change in muscle sympathetic nerve activity (MSNA) at 3-month follow-up. The effects of baseline MSNA and change in MSNA over time on mortality in the main study were also assessed.
Results
40 patients with HFrEF were included in this analysis (age 71.3±11.7 years, LVEF 34.2±7.7%, 57.5% in New York Heart Association (NYHA) Functional Class II, 42.5% in NYHA Functional Class III, AHI 35.2±11 events·h−1). Sympathetic tone evolution during follow-up did not differ between groups (controls: 47.6±8.3 bursts·min−1 at baseline to 44.6±11.2 bursts·min−1; ASV group: 43.0±9.0 bursts·min−1 at baseline to 42.74±9.45 bursts·min−1). The reduction in sympathetic tone was associated with significantly increased cardiovascular mortality in the ASV group, whereas in the control group reduced sympathetic tone appeared to be protective.
Conclusions
Suppression of CSA with ASV did not seem to have a significant effect on chronic heart failure-related sympathetic activation. Simultaneous suppression of CSA and reduction in MSNA was associated with increased cardiovascular mortality.
- Share
- Share on Facebook
- Share on X
- Share on LinkedIn