Jean-Benoît Martinot, Nhat-Nam Le-Dong, Renaud Tamisier, Sébastien Bailly, Jean-Louis Pépin
- Share
- Share on Facebook
- Share on X
- Share on LinkedIn
Abstract
Background
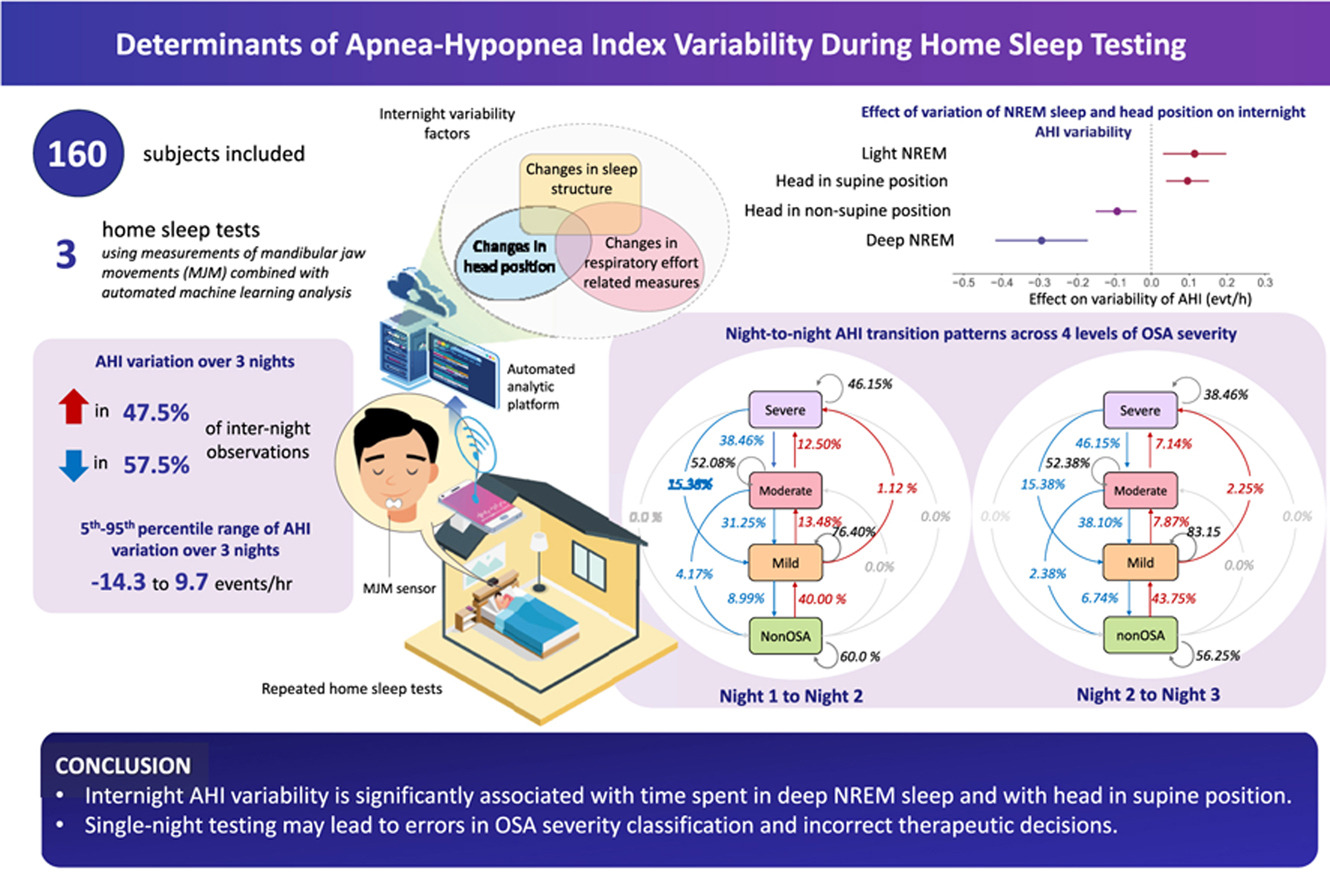
A single-night attended in-laboratory polysomnography or home sleep testing are common approaches for obstructive sleep apnea (OSA) diagnosis. However, internight variability in apnea-hypopnea index value is common, and may result in misclassification of OSA severity and inapropriate treatment decisions.
Objective
To investigate factors determining short-term apnea-hypopnea index variability using multi-night automated home sleep testing, and to determine how this variability impacts clinical decisions.
Patients/methods
Adults with suspected OSA who successfully performed three home sleep tests using measurements of mandibular jaw movements (Sunrise, Namur, Belgium) combined with automated machine learning analysis were enrolled. Data analysis included principal component analysis, generalized estimating equation regression and qualitative agreement analysis.
Results
160 individuals who performed three sleep tests over a mean of 8.78 ± 8.48 days were included. The apnea-hypopnea index varied by −0.88 events/h (5th-95th percentile range: −14.33 to 9.72 events/h). Based on a single-night recording, rates of overtreatment and undertreatment would have been of 13.5% and 6.0%, respectively. Regression analysis adjusted for age, sex, [body mass index], total sleep time, and time between home sleep tests showed that time spent in deep non-rapid eye movement sleep and with head in supine position were independent significant predictors of the apnea-hypopnea index variability.
Conclusions
At the individual level, short-term internight variability in the apnea-hypopnea index was significantly associated with time spent in deep non-rapid eye movement sleep and head in supine position. Clinical decisions based on a single-night testing may lead to errors in OSA severity classification and incorrect therapeutic decisions.
- Share
- Share on Facebook
- Share on X
- Share on LinkedIn